Falsified medicines


IFPMA and our members are playing our part in driving a long-term, sustainable, multi-pronged strategy to fight the extremely serious threat of falsified medicines to global public health.
Overview
The WHO defines falsified medicines as “medical products that deliberately/fraudulently misrepresent their identity/composition or source.”
No quality falsified medicines exist. Manufacturing, distributing, and selling falsified medicines is a crime. We are at the forefront of the battle against falsified medicines that put the lives of people in every country needing medical products in danger.
The growing threat from falsified medicines
According to the Pharmaceutical Security Institute (PSI), pharmaceutical crime incidents are up 38% from 2020. Brand-name, generic, prescription, or over the counter medicines can all be falsified. Although counterfeiters often target lifestyle drugs, life-saving medicines are the fastest growing category of falsified medicines.
IFPMA acts against falsified medicines with vigor, and we campaign to persuade governments and the public to join us in action. Our members work closely with regulatory and enforcement officials, local authorities, and international bodies.
Falsified medicines put patients at great risk of being harmed or failing to receive the treatment they need. They can trigger additional illness, disability, resistance to authentic medicines, and even death.
countries have been impacted by pharmaceutical crime, including falsified, diverted, or stolen pharmaceuticals
medicinal products circulating in low-and middle-income countries is either substandard or falsified
therapeutic categories have had falsified medicines found within them
Analysis of falsified medicines found samples that contained no active pharmaceutical ingredient (API), or even worse, contained the wrong API, the wrong dosage, or other dangerous substances.
On top of this, falsified medicines undermine patients’ trust in health systems, government agencies, health care providers, and manufacturers of genuine medicines.
A global risk
Falsified medicines can be manufactured everywhere. But they travel and are sold more easily in countries where they can move across borders with less risk of detection and a country’s regulatory system is weak or non-existent.
While this is an issue worldwide, Africa is particularly at risk, with the greatest prevalence of falsified medicines.
A study published in The American Journal of Tropical Medicine and Hygiene found that 52.8% of all counterfeit medicines detected in the legitimate supply chain are life-saving-related treatments.
Once falsified medicines enter the supply chain, they endanger lives across the globe. This international threat is magnified by the growing online market for falsified medicines.
Fighting falsified medicines
Although companies are investing considerably in protecting their product, it is essential that countries strengthen legislative and enforcement frameworks.
In addition, we need far greater consistency, standardization, and robust data collection for analysis, better reporting by countries, and more detail in those reports.
Defining falsified medicines
The WHO defines falsified medicines as “medical products that deliberately/fraudulently misrepresent their identity/composition or source.
Intention to deceive is the key distinction between substandard and falsified medicines.
A substandard medicine is approved and legally manufactured but does not meet all quality criteria. Even though it may pose a significant health risk, it shouldn’t be regarded as falsified.
But falsified medicines are also, by definition, likely to be substandard.
As defined by the WHO Member States Mechanism, the term falsified can be used “when the authorized manufacturer deliberately fails to meet these quality standards or specifications due to misrepresentation of identity, composition, or source…”
IFPMA agrees with the WHO definition which is in line with our position, as stated in our Ten Principles.
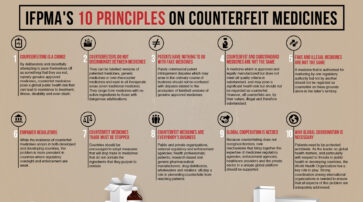
IFPMA’s 10 principles on counterfeit medicines
The International Federation of Pharmaceutical Manufacturers and Associations (IFPMA) published its “Ten Principles on Counterfeit Medicines” to draw public attention to the issue.
Read moreA collective fight
IFPMA is at the forefront of a collective, integrated, multi-stakeholder fight against the complex health challenge of falsified medicines.
An effective response to the threat of falsified medicines demands collaboration by all stakeholders including patients, public health professionals, public and private organizations, pharmaceutical distributors, wholesalers, retailers, national regulatory and enforcement agencies, and the WHO.
It calls for strong national regulatory frameworks, effective legislation, robust awareness, and the prevention, control, detection, and monitoring of falsified medicines.

Illegal online pharmacies
The internet is a growing global marketplace for falsified medicines.
Illegal websites are a major obstacle to stamping out falsified medicines: 50% of medicines sold online by pharmacy websites that hide their physical street address are fake and 89% of illegal online pharmacies don’t require a prescription. Tens of thousands of illegal websites sell unsafe and poor quality medicines, while pretending to be legitimate pharmacies.
It’s vital for governments to strengthen laws and enforcement tools to address the growing number of illegitimate online pharmacies. They should also develop robust awareness programs about the dangers of purchasing falsified medicines online while also offering advice on how to buy safe medicines from lawful sources.
In the meantime, initiatives such the Alliance for Safe Online Pharmacies in the EU and US and CSIP (Center for Safe Internet Pharmacies) are already raising public awareness and inviting authorities to “evaluate policies and legal measures to tackle illegal online sales.”

Building strong national regulatory frameworks
The WHO has spotlighted weak or non-existent national regulatory systems as a key factor encouraging criminals to falsify medicines.
IFPMA and our members play a significant and dynamic role in strengthening regulatory systems, so they’re better equipped to prevent falsified medicines from endangering people’s health and well-being.
To fight the threat and promote best practices, we have organized workshops on falsified medicines featuring leading international and regional experts and thought leaders. Representatives from national regulatory authorities, regional intergovernmental organizations, international organizations, non-governmental organizations, and the private sector took part.
Our members actively share expertise with regulatory and enforcement officials around the world. They work closely with local authorities and international bodies to improve how falsified medicines are identified, collect information and develop more effective ways of dealing with suspected falsifiers.

Implementing effective technologies
Identification and traceability tools are extremely valuable methods of securing the legal supply chain for medical products.
They enable medical products to be tracked forward through specific stages of the extended supply chain.
The innovative pharmaceutical industry has built pioneering serialization/traceability capabilities and expertise, which can be helpful in certain contexts.
When it comes to planning how to implement a product identification or traceability system, IFPMA advocates for:
- Harmonized standards
- Strategic planning
- A stepwise approach
- An implementation framework
- Early stakeholder engagement.
These five principles are described in more detail here.
Tough, appropriate measures
Dealing in falsified medicines is currently easy, cheap, and lucrative, with a low risk of being caught or punished.
If criminals are caught, the punishment for falsifying medicines doesn’t come close to reflecting the severity of the crime.
Fortunately, some authorities are taking measures to deal with falsified medicines that are, for the first time, appropriately tough. The Medicrime Convention is chief among them.
The Medicrime Convention
IFPMA is an observer to the Medicrime Convention drawn up by the Council of Europe, the first international treaty against counterfeit medical products and similar crimes involving threats to public health.
It helps enable effective prosecution, seizes proceeds from falsification, and ensures national and international cooperation to fight this crime.
The convention establishes as criminal offenses:
- Manufacturing counterfeit medical products
- Supplying, offering to supply, and trafficking in counterfeit medical products
- Falsifying documents
- Unauthorized manufacturing or supplying of medicinal products and placing medical devices on the market that do not comply with conformity requirements.
Raising awareness
Public awareness and education are vital to addressing the impact of falsified medicines.
Effective awareness campaigns equip patients with the knowledge to help avoid this threat and safeguard their own health. But many patients around the globe have not received information about the threat of falsified medicines and the resulting health risk.
IFPMA helps inform patients and the global population about the risk posed by falsified medicines. We have developed impactful educational materials in partnership with like-minded organizations, which are designed to build productive awareness and avoid sensational claims.
Support the Medicrime Convention
We invite governments to join and ratify the unique Medicrime Convention